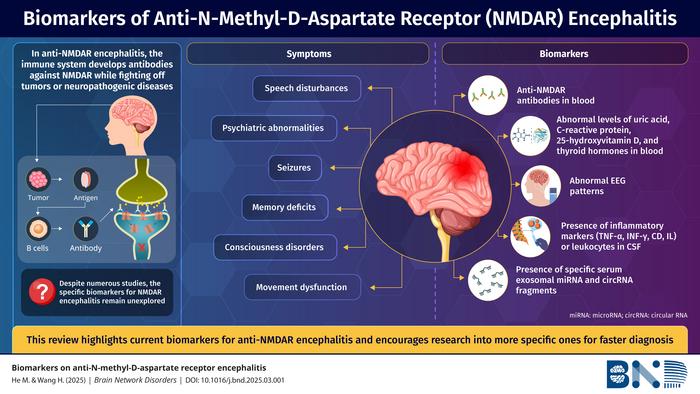
A new peer-reviewed review in Brain Network Disorders consolidates current evidence on clinical features, mechanisms, and laboratory biomarkers that can aid diagnosis and monitoring of anti-N-methyl-D-aspartate receptor (anti-NMDAR) encephalitis, a leading form of autoimmune encephalitis in children and young adults.
Why it matters
Anti-NMDAR encephalitis presents with neuropsychiatric symptoms and seizures, yet timely diagnosis can be challenging when antibody assays are negative or inconclusive. By organizing the best-supported biomarkers across serum, cerebrospinal fluid (CSF), EEG, and emerging molecular assays, the review offers a practical roadmap for clinicians and researchers to refine work-ups and stratify care. :contentReference[oaicite:0]{index=0}
The study at a glance
- Authors: Minchao He and Honghao Wang, The Second Affiliated Hospital of South China University of Technology (Guangzhou, China).
- Publication: Online 13 May 2025; Volume 1, Issue 2 (June 2025) of Brain Network Disorders. Open access. DOI: 10.1016/j.bnd.2025.03.001.
- Method: Narrative literature review synthesizing clinical phenotypes, pathophysiology, and biomarker evidence relevant to anti-NMDAR encephalitis.
Clinical phenotype and triggers
The review summarizes eight hallmark symptom domains: psychiatric abnormalities, seizures, memory deficits, consciousness disturbance, movement disorder, autonomic dysregulation, speech disturbance, and central hypoventilation. Reported triggers include tumors (notably ovarian teratoma), viral infections, and post-vaccination cases, aligning with prior literature on antibody-mediated synaptic disorders.
Key biomarker takeaways
- Primary test: Detect anti-NMDAR (GluN1) IgG in CSF and serum—CSF generally offers higher sensitivity and pathogenic relevance.
- If antibodies are negative/low: Supportive indicators may include serum uric acid, C-reactive protein, 25-hydroxy-vitamin D, and thyroid function markers; abnormalities can strengthen clinical suspicion when interpreted alongside phenotype.
- Neurophysiology: EEG abnormalities (including network-level changes) can act as accessible functional biomarkers during acute and convalescent phases. {index=8}
- CSF cytokines/chemokines: Interleukin and chemokine profiles, when available, may help characterize inflammatory activity and track response.
- Emerging molecular markers: MicroRNAs, circular RNAs, and other transcriptomic signatures are under active study for diagnosis and disease monitoring.
Implications for practice
The authors advocate a stepwise approach: prioritize CSF/serum anti-NMDAR antibody testing, then layer supportive laboratory indices and EEG when clinical suspicion remains high, and consider advanced CSF and molecular assays where available. This structured pathway may shorten time to immunotherapy and improve outcomes, while ongoing research clarifies which biomarkers most reliably predict severity and recovery.