EARLY STATUS EPILEPTICUS
0-5 Minutes
- Assess and support Airway and Breathing as required Apply high flow oxygen, attach monitoring, Finger-prick glucose, obtain IV access
1-5 Minutes
- If IV access established
- Lorazepam: 0.1 mg/kg IV (MAX 4MG / DOSE), may repeat in 5–10 min
- If IV access not established
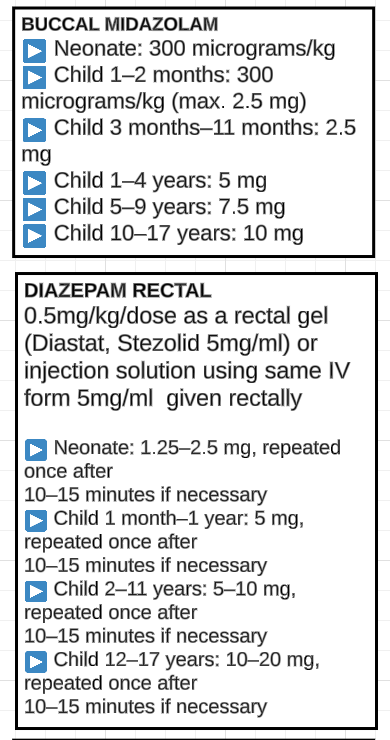
- Buccal Midazolam 0.5mg/kg (max 10mg) OR
Rectal Diazepam: 0.5 mg/kg PR (Max 20mg) Neonate: 300 micrograms/kg
- Child 1–2 months: 300 micrograms/kg (max. 2.5 mg)
- Child 3 months–11 months: 2.5 mg
- Child 1–4 years: 5 mg
- Child 5–9 years: 7.5 mg
- Child 10–17 years: 10 mg
- OR Midazolam IM: 5 mg if 13–40 kg, 10 mg if >40 kg (0.3 mg/kg up to 10 mg)
- OR Midazolam Intranasal: 0.2 mg/kg
- Buccal Midazolam 0.5mg/kg (max 10mg) OR
Rectal Diazepam: 0.5 mg/kg PR (Max 20mg) Neonate: 300 micrograms/kg
ESTABLISHED STATUS EPILEPTICUS
 15 Minutes
15 Minutes
- If IV access established
- Lorazepam: 0.1 mg/kg IV (MAX 4MG / DOSE)
- If IV access not established
- Buccal Midazolam 0.5mg/kg (max 10mg) OR
- Midazolam Intranasal: 0.2 mg/kg OR
- If Diazepam second dose needed give 0.25mg/kg
25 Minutes
- Patient Not Already on Phenytoin
- Phenytoin 20 mg/kg IV/IO (GIVE OVER 20 MINUTES; RISK OF EXTRAVASATION)
OR
- PHENTYOIN is only compatible in saline and the IV contains propylene glycol. Fosphenytoin is compatible in saline, dextrose, and ringer lactate
- Levetiracetam 30mg/kg IV/IO (max 3g) over 5-10 minutes OR
- Phenobarbital 20 mg/kg IV (Give over 5 minutes)(may give an additional 5–10 mg/kg) OR
- Lacosamide 10mg/kg IV with a total daily dose of up to 15mg/kg if still seizing and PR interval </= 200ms OR
- Sodium Valproate 20mg/kg IV AVOID IF SUSPECTED METABOLIC CONDITION
- Phenytoin 20 mg/kg IV/IO (GIVE OVER 20 MINUTES; RISK OF EXTRAVASATION)
OR
- Patient Already on Phenytoin
- Levetiracetam 30mg/kg IV/IO (max 3g) over 5-10 minutes OR
- Phenobarbital 20 mg/kg IV (Give over 5 minutes) OR
- Lacosamide 10mg/kg IV with a total daily dose of up to 15mg/kg if still seizing and PR interval </= 200ms OR
- Sodium Valproate 20mg/kg IV ( AVOID IF SUSPECTED METABOLIC CONDITION)
REFRACTORY STATUS EPILEPTICUS
45 Minutes
- Rapid sequence induction of anaesthesia: intubate and ventilate Propofol 2-4mg/kg IV (unless suspected or known metabolic condition or child on ketogenic diet) OR
- thiopental 3-5mg/kg IV Short acting muscle relaxant (not infusion)
EEG monitoring should be initiated 15–60 min after seizure onset to evaluate for non-convulsive status epilepticus for patients who are not returning to baseline within 10 min of convulsive seizure cessation or within 60 min for patients in whom ongoing seizures are suspected
60 Minutes
- Reassess and consider CT if focal signs, focal/atypical seizure, trauma, possible raised ICP Check sodium, magnesium, calcium and ammonia results Specific therapies as appropriate: antibiotics, aciclovir, neurosurgery, etc If intubated for hypoventilation, assess for extubation. Lumbar puncture should not be performed in child with reduced GCS
- If still seizing
- STEP A
- Load with Levetiracetam 30mg/kg IV (max 3 grams) over 5 minutes (if not used already)
- Aim to terminate seizures within 30 minutes with midazolam infusion.
- Bolus Midazolam 0.1mg/kg & start infusion at 2 micrograms/kg/minute (wait 10 minutes).
- Increase Midazolam rate to 5, 10, 15, 20 micrograms/kg/minute every 5 min until seizure stopped (titrated as needed to achieve clinical or electrographic seizure suppression or EEG burst-suppression) . DO NOT bolus on increments as escalation rapid Monitor for hypotension.
- Avoid muscle relaxation (masks seizures) Re-load with ½ dose (10 mg/kg) phenytoin OR
- 10 mg/kg phenobarbitone Ongoing seizures discuss urgently with PICU consultant and Neurology Consultant
- If still seizing
- STEP B
- Pentobarbital initial loading dose of 5–15 mg/kg (followed by another 5–10 mg/kg if needed) followed by an infusion at 0.5–5 mg/kg/hour titrated as needed to achieve seizure suppression orEEG burst-suppression OR
- PROPOFOL initial 1–2 mg/kg loading dose and initial 20 mcg/kg/minute infusion titrated up by about 5–10 mcg/kg/minute as needed, with caution advised with dosing above 65 mcg/kg/minute NOT IF CHILD IS ON KETOGENIC DIET OR
- Thiopentone infusion OR
- STEP C
- Volatile anaesthesia
Institute specific antiepileptic drugs while the continous infusions are being weaned. In previously well child consider FIRES (Febrile infection related epilepsy syndrome) OR autoimmune conditions
- Volatile anaesthesia
Continue 24–48 h of electrographic seizure control before slowly withdrawing the continous infusions over 6 to 12 hours. Seizures may recur despite EEG-confirmed burst suppression or complete suppression of background seizures. Review electrographic recordings twice daily.
SUPER REFRACTORY STATUS EPILEPTICUS
- Repeat Steps ABC
- Ketamine infusion initial bolus of 2–3 mg/kg followed by continuous infusion of 10 µg/kg/min, increasing the infusion rate by 5–10 µg/kg/min every 10 min up to a maximum of 100 µg/kg/min, with every increment being preceded by a bolus of 1–2 mg/kg
- Methylprednisolone (1 g/d for 3-5 days ± tapering oral steroids)
- Immunoglobulins (0.5 g/kg/d for 4 days ) 0R Plasmapheresis
- Magnesium infusion (2-6 g/h to obtain serum level of 3.5 mmol/L)
- Pyridoxine (in children under 2 years (30mg/kg/day IV infusion))
- Consider induced hypothermia, ketogenic diet, epilepsy surgery
- Consider weaning anaesthesia on days 3-5.
- If breakthrough seizures repeat anaesthesia cycles again

